This condition has emerged as one of the most controversial topics in musculoskeletal medicine and rehabilitation[3]. This controversy extends to almost every aspect of the pathology including the definition, incidence, pathoanatomical contributions, diagnosis, and treatment.
The term ‘TOS’ does not specify the structure being compressed. Investigators namely identify two main categories of TOS: the vascular form (arterial or venous), which raises few diagnostic problems, and the neurological form, which occurs in more than 95-99% of all cases of TOS. Therefore the syndrome should be differentiated by using the terms arterial TOS (ATOS), venous TOS (VTOS) or neurogenic (NTOS).
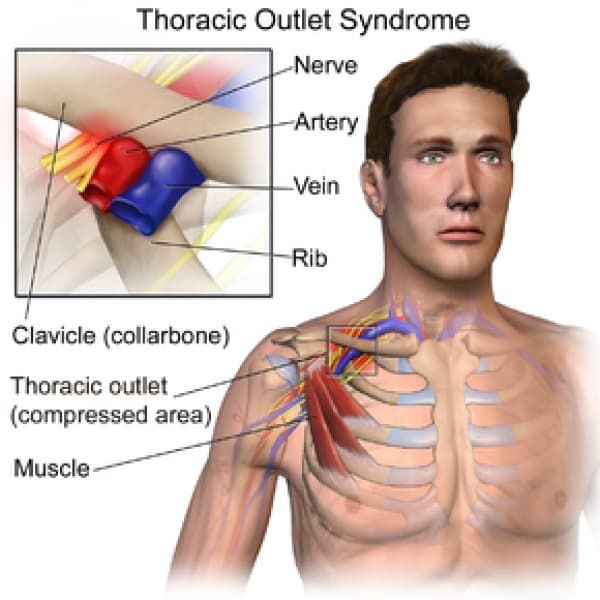
Clinically Relevant Anatomy
The first narrowing area is the most proximal and is named the interscalene triangle: This triangle is bordered by the anterior scalene muscle anteriorly, the middle scalene muscle posteriorly, and the medial surface of the first rib inferiorly. The presence of the scalene minimus muscle and the fact that both the anterior and middle scalene muscles have their insertion in the first rib (which can cause overlapping) can cause a narrow space and therefore compression . The brachial plexus and the subclavian artery pass through this space.
The second passageway is called the costoclavicular triangle which is bordered anteriorly by the middle third of the clavicle, posteromedially by the first rib, and posterolaterally by the upper border of the scapula. The subclavian vein, artery and plexus brachialis crosses this costoclavicular region and then further enters the subcoracoïd space. Just distal to the insterscalene triangle. Compression of these structures can occur as a result of congenital abnormalities, trauma to the first rib or clavicle, and structural changes in the subclavian muscle or the costocoracoid ligament.
The last passageway is called the subcoracoid or sub-pectoralis minor space: This last passageway is beneath the coracoid process just under the pectoralis minor tendon. The borders of the thoraco-coraco-pectoral space include the coracoid process superiorly, the pec minor anteriorly, and ribs 2-4 posteriorly. Shortening of the Pectoralis Major can lead to a narrowing of this last space and therefore compression of the neurovascular structures during hyperabduction.
Certain anatomical abnormalities can be potentially compromising to the thoracic outlet as well. These include the presence of a cervical rib, congenital soft tissue abnormalities, clavicular hypomobility , and functionally acquired anatomical changes[4]. Soft tissue abnormalities may create compression or tension loading of the neurovascular structures found within the thoracic outlet (such as hypertrophy , a broader middle scalene attachment on the 1st rib or fibrous bands that increase the stiffness,…).
Epidemiology/Etiology
TOS affects approximately 8% of the population and is 3-4 times as frequent In woman as in men between the age of 20 and 50 years. Females have less-developed muscles, a greater tendency for drooping shoulders owing to additional breast tissue, a narrowed thoracic outlet and an anatomical lower sternum, these factors change the angle between the scalene muscles and consequently cause a higher prevalence in women. The mean age of people effected with TOS is 30s-40s; it is rarely seen in children. Almost all cases of TOS (95-98%) affect the brachial plexus; the other 2-5% affecting vascular structures, such as the subclavian artery and vein.
There are several factors which can cause TOS: Cervical ribs are present in approximately 0.5-0.6% of the population, 50-80% of which are bilateral, and 10-20% produce symptoms; the female to male ratio is 2:1. Cervical ribs and the fibromuscular bands connected to them are the cause of most neural compression. Fibrous bands are a more common cause of TOS than rib anomalies.
Congenital Factors:
- Cervical rib
- Prolonged transverse process
- Anomalous muscles
- Fibrous anomalies (transversocostal, costocostal)
- Abnormalities of the insertion of the scalene muscles
- Fibrous muscular bands
- Exostosis of the first rib
- Cervicodorsal scoliosis
- Congenital uni- or bilateral elevated scapula
- Location of the A. or V. Subclavian in relation to the M. scalene anterior
Acquired Conditions: - Postural factors
- Dropped shoulder condition
- Wrong work posture (standing or sitting without paying attention to the physiological curvature of the spine)
- Heavy mammaries
- Trauma
- Clavicle fracture
- Rib fracture
- Hyperextension neck injury, whiplash
- Repetitive stress injuries (repetitive injury most often form sitting at a keyboard for long hours)
Muscular Causes:
- Hypertrophy of the scalene muscles
- Decrease of the tonus of the M. trapezius, M. levator scapulae, M.rhomboids
- Shortening of the scalene muscles, M. trapezius, M. levator scapulae, pectoral muscles
Characteristics/Clinical Presentation
Signs and symptoms of thoracic outlet syndrome vary from patient to patient due to the location of nerve and/or vessel involvement. Symptoms range from mild pain and sensory changes to limb threatening complications in severe cases.
Patients with thoracic outlet syndrome will most likely present pain anywhere between the neck, face and occipital region or into the chest, shoulder and upper extremity and paresthesia in upper extremity. The patient may also complain of altered or absent sensation, weakness, fatigue, a feeling of heaviness in the arm and hand. The skin can also be blotchy or discolored. A different temperature can also be observed.
Signs and symptoms are typically worse when the arm is abducted overhead and externally rotated with the head rotated to the same or the opposite side. As a result activities such as overhead throwing, serving a tennis ball, painting a ceiling, driving, or typing may exacerbate symptoms.
When the upper plexus (C5,6,7) is involved there is pain in the side of the neck and this pain may radiate to the ear and face. Often the pain radiates from the ear posteriorly to the rhomboids and anteriorly over the clavicle and pectoralis regions. The pain may move laterally down the radial nerve area. Headaches are not uncommon when the upper plexus is involved.
Patients with lower plexus (C8,T1) involvement typically have symptoms which are present in the anterior and posterior shoulder region and radiate down the ulnar side of the forearm into the hand, the ring and small fingers.
There are four categories of thoracic outlet syndrome and each presents with unique signs and symptoms (see Table 1). Typically TOS does not follow a dermatomal or myotomal pattern unless there is nerve root involvement, which will be important in determining your PT diagnosis and planning your treatment
Differential Diagnosis
Due the it's variability, TOS can be difficult to tease out from other pathologies with similar presentations. A thorough history and evaluation must be done to determine if the patient’s symptoms are truly TOS. The following pathologies are common differential diagnosis for TOS :
- Carpal tunnel syndrome
- De Quervain’s tenosynovitis
- Lateral epicondylitis
- Medial epicondylitis
- Complex regional pain syndrome (CRPS I or II).
- Horner’s Syndrome
- Raynaud’s disease
- Cervical disease (especially discogenic)
- Brachial plexus trauma
- Systemic disorders: inflammatory disease, esophageal or cardiac disease
- Upper extremity deep venous thrombosis (UEDVT), Paget-Schroetter syndrome
- Rotator cuff pathology
- Glenohumeral joint instability
- Nerve root involvement
- Shoulder Instability
- Malignancies (local tumours)
- Chest pain, angina
- Vasculitis
- Thoracic (T4) syndrome
- Sympathetic-mediated pain
Systematic causes of brachial plexus pain include:
- Pancoast’s Syndrome
- Radiation induced brachial plexopathy
- Parsonage Turner Syndrome
There are conditions that can coexist with TOS. It is important to identify these conditions because they should be treated separately. These associated conditions include: - carpal tunnel syndrome
- peripheral neuropathies (like ulnar nerve entrapment at the elbow, shoulder tendinitis and impingement syndrome)
- fibromyalgia of the shoulder and neck muscles
- cervical disc disease (like cervical spondylosis and herniated cervical disk)
Outcome Measures
DASH (Disability of Arm Shoulder and Hand)
SPADI (Shoulder Pain And Disability Index)
NPRS (Numeric Pain Rating Scale)
McGill Pain Questionnaire
Diagnostic Procedures
The diagnosis of TOS is essentially based on history, physical examination, provocative tests, and if needed ultrasound, radiological evaluation and electrodiagnostic evaluation. It must always kept in mind that TOS diagnosis is usually confirmed by elimination of other causes with similar clinical presentation. Especially differential diagnosis of cervical radiculopathies and upper extremity entrapment neuropathies can be hard (McGillicuddy 2004). In order to diagnose accurately, the clinical presentation must be evaluated as either neurogenic (compression of the brachial plexus) or vascular (compression of the subclavian vessels). TOS manifestations are varied and there is no single definitive test, which makes it difficult to diagnose.