Anatomy and Pathological Process
The knee joint consists of both approximation of the proximal tibia and the distal end of the femur. The cartilage located on the ends of the femur and tibia contain an extra cellular matrix that contains type 2 protoglycans that function by drawing fluid into the joint causing increased shock absorption and proper joint nutrition. There is some evidence to support that as the ageing process occurs the type 2 collagen fibers decrease in size and therefore less fluid an nutrition gets into the joint surfaces eventually leading to decreased protection along boney surfaces.
The knee (art. genus) is a synovial joint, which consists of 3 articulations. The primary joint, art. tibiofemoral, is located between the convex femoral condyles and the concave tibial condyles. There is also the art. patellofemoralis between the femur and the patella and the art. tibiofibularis located between the tibia and fibula. OA can only occur in the two primary articulations of the knee, namely the tibiofemoral and patellofemoral joint, because they have to sustain more motion than the art. tibiofibularis.
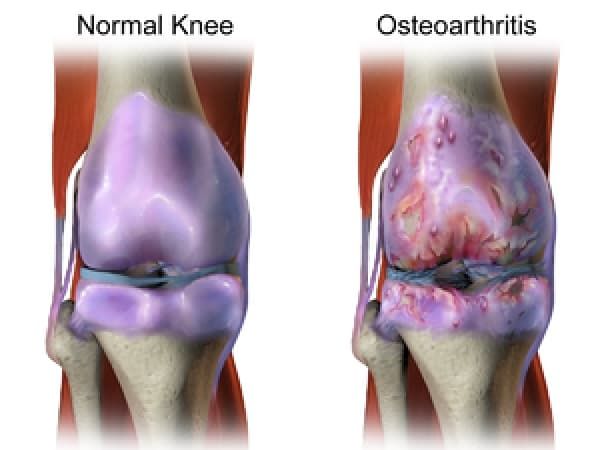
“The pathogenesis of knee OA have been linked to biomechanical and biochemical changes in the cartilage of the knee joint.” (Kirstin Uth et al, 2014) The cartilage ensures that the bone surfaces can move painless and with low friction to each other. In OA, the cartilage decreases in thickness and quality, it becomes thinner and softer, cracks may occur and it will eventually crumble off. Cartilage that has been damaged, cannot recover. Finally the cartilage will disappear. The bone surfaces can also be affected, the bone will expand and spurs (osteophytes) will develop.
Not only the cartilage can be affected, there can also occur laxity of the ligaments and muscle atrophy.
Epidemiology/Etiology
Osteoarthritis is the most prevalent form of arthritis and occurs especially in the knee joint. It affects nearly 6% of all adults, but more women are affected than men. “According to a number of published reports, anywhere from 6% to over 13% of men, but between 7% and 19% of women, over 45 years of age are affected, resulting in a 45% less risk of incidence in men (Coleman, et al).”
Age is a determining factor in the development of OA. “As the population ages in demographic terms, the prevalence of OA is expected to rise (Coleman, et al).” From the age of 40 there is an increased risk of OA. Approximately 50% of the 65+ population are affected by OA in the knee, but it can also affect young people.
Age is not the only factor that plays a role in the evolution of OA. Other risk factors are:
- Obesity
- Joint hypermobility or instability
- Sport stress with high impact loading
- Repetitive knee bending or heavy weight lifting
- Specific occupations
- Peripheral neuropathy
- Injury to the joint
- History of immobilisation
- Family history
Characteristics/Clinical Presentation
Signs of knee osteoarthritis are pain at beginning of the movement, later on pain during movement and eventually permanent pain. These patients will also experience a loss of function like stiffness, decreased range of motion (ROM) and impairment in everyday activities. Other possible characteristics of knee OA are bony enlargement, crepitus, joint-line tenderness and elevated sensitivity to cold and/or damp.[14]
We can subdivide knee osteoarthritis in 5 stages:
- Stage 0: This is the “normal” knee health, without any pain in the joint functions.
- Stage 1: A person in this stage has very minor bone spur growth and is not experiencing any pain or discomfort.
- Stage 2: This is the stage where people will experience symptoms for the first time. They will have pain after a long day of walking and will sense a greater stiffness in the joint. It is a mild stage of the condition, but X-rays will already reveal greater bone spur growth. The cartilage will likely remain at a healthy size.
- Stage 3: Stage 3 is considered as a moderate osteoarthritis. People with this stage will experience a frequent pain during movement. The joint stiffness will also be more present, especially after sitting for long periods and in the morning. The cartilage between the bones shows obvious damage, and the space between the bones is getting smaller.
- Stage 4: This is the most severe stage of osteoarthritis. The joint space between the bones will be dramatically reduced, the cartilage will almost be completely gone and the synovial fluid will be decreased. That is why people will experience lots of pain and discomfort during walking or moving the joint.
Diagnosis
The diagnosis can be established by clinical examination, and it can be confirmed by X-rays. The main characteristics are changes in the subchondral bone, joint space narrowing, subchondral sclerosis, subchondral cyst formation and osteophytes. In early stage of osteoarthritis, the results of the radiography can show a minimal unequal joint space narrowing. If it deteriorates you still find the same problems, but the patient experiences a lateral subluxation of the tibia as well. If it deteriorates more, the joint line will disappear completely. The image shows that the medial joint space is more narrow than the lateral joint space.