In a typical monthly menstrual cycle, endometrial cells lining the uterine walls are stimulated through a release of hormones and multiply in order to provide an ideal environment for egg fertiliztion. If fertilization of the egg does not occur, the uterus sloughs off the lining of blood (endometrial tissue) and menstrual flow occurs for 3 to 5 days.
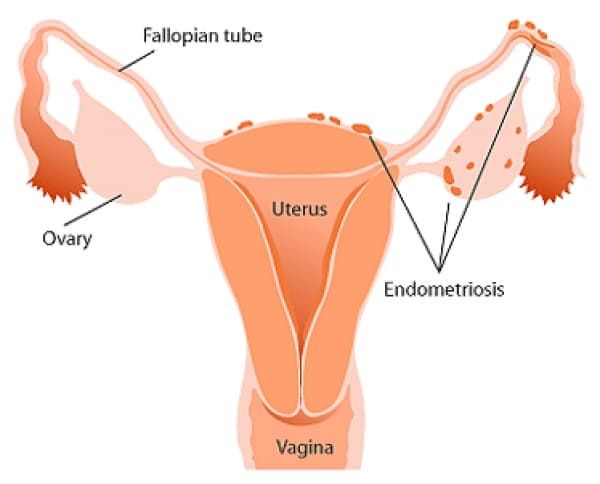
When affected by endometriosis, endometrial tissue is misplaced outside the uterus in various places. Despite the location of the tissue, the same monthly menstrual cycle occurs. The misplaced tissue engorges with blood, as it would in the uterine lining. Since this blood has no course to drain out of the vagina it remains where it is resulting in "chocolate cysts" wherever endometrial cells are located. In addition to cysts, trapped blood may lead to scar tissue, adhesions and irritation of the surrounding tissue which causes pelvic pain and fertility problems.
Blood deposits or ectopic implantation may occur anywhere in the body but most commonly affects the ovaries, fallopian tubes, broad ligaments, bladder, pelvic musculature, perineum, vulva, vagina, or intestines. It has been discovered that endometrial tissue has the ability to migrate through the body, and, in less common cases, has been found in the abdominal cavity, kidneys, small bowel, appendix, diaphragm, pleura, bone and even the brain.
Prevalence
The incidence of Endometriosis has been on the rise in Western countries for the last 40 to 50 years. Although there are statistics in the literature, the true prevalence of endometriosis is unknown because many women remain asymptomatic. It has been reported that endometriosis occurs in a wide range of 7%- 60% of all women. Further Reports in 2008 revealed that endometriosis occurs in 7%-10% of women in the general population, 2%-50% of women suffering from infertility, and 71%-87% of women with chronic menstrual pain. Unlike many common disorders, there have been no correlations between endometriosis and specific populations. Endometriosis has been shown to affect women of all race, cultures, ethnic origins, socioeconomic status, and geographic backgrounds.
Characteristics/Clinical Presentation
Generally, endometriosis becomes apparent soon after menses begins in early teen years, and symptoms continue until menopause. Although any woman of child-bearing age is at risk of developing Endometriosis, it is more common in those who have postponed pregnancy.
Endometriosis has been shown to vary in its degree of severity. In order to gauge the level of severity, the American Society of Reproductive Medicine has developed five stages of classification: I (minimal), II (mild), III (moderate), IV (severe), V (extensive). Despite these classifications, symptoms do not always correlate with disease severity. Many women with severe endometriosis have little pain or remain asymptomatic, while some with minimal or mild classification may experience intense symptoms affecting quality of life. It is likely that if gone untreated, symptoms will progress and worsen over time.
Common Sign and Symptoms
- Abdominal pain, fatigue and mood change beginning 1-2 days before menstruation and continuing for the duration
- Constant/intermittent, or cyclical pelvic and/or low back pain (unilateral or bilateral)
- Infertility - often first diagnosed in women who are seeking treatment for infertility
- History of ectopic pregnancy or miscarriage
- Dysmenorrhea (painful menstruation) - commonly identified as the chief complaint if implants are located over the uterosacral ligaments
- Dyspareunia (painful intercourse) - local adhesions may be irritated by penile penetration
- Painful defecation - adhesions may be present over the large bowel. As faecal matter moves through the intestines these adhesions can be stretched causing local irritation.
- Low-grade fever
- Diarrhoea, constipation, rectal bleeding
- Referred pain to the low back/sacral groin, posterior leg, upper abdomen, or lower abdominal.suprapubic areas
- Menorrhagia/menometrorrhagia - excessive or occasional heavy periods may be experienced, along with bleeding between periods
Less Common Signs and Symptoms
- Chest pain/hemoptysis - due to endometrial implants in the lungs
- Headache/seizures - due to endometrial implants in the brain
Associated Co-morbidities
- Several health problems have been shown to exist in combination with endometriosis.
- A large percentage of women experience co-morbidities such as:
- Fibromyalgia
- Hypothyroidism
- Chronic fatigue syndrome
- Allergies
- Asthma
- Rheumatoid arthritis
- Multiple sclerosis
- Systemic lupus erythematosus
- Auto-immune disorders
Medications
- Anti Inflammatories (NSAIDs)- Over the counter or prescribed NSAIDs work by decreasing the pain and amount of inflammation in the region of disease caused by displaced endometrial tissue or scaring. NSAIDs also decrease pain associated with menstrual bleeding by blocking the protein prostaglandin.
- Birth Control Hormones- creates hormone levels in the body similar to those during pregnancy. This may slow or cease the growth of endometrial implants, and stop the shedding and discharge of menstrual fluid which will lead to a decrease in pain. This treatment may be used in the form of a pill, patch or ring and has been shown to have the least amount of side effects.
- Gonadotropin Releasing Hormone Agonist (GnRH-a)- This form of hormone treatment lowers estrogen levels in the body producing a state which mimics menopause. Typically this form of treatment is utilized in more severe cases where the pain is not relieved by birth control hormones and NSAIDs. GnRH-a works by stopping the growth-shrinking implants which in turn reduces pain.
- Progestin (pill or shot) - This form of hormone therapy works to create levels of progestin in the body similar to pregnancy. By mimicking the hormonal characteristics of pregnancy ovulation ceases and estrogen levels lower which causes shrinkage of endometrial growths and reduced pain.
- Danazol - Increases androgen levels and decreases estrogen levels to create a menopause-like state. Similar to previous hormone therapy, this shrinks and stops the growth of endometrial implants which typically reduces pain. Treatment effects last approximately 6-12 weeks and may produce adverse signs/symptoms.
- Aromatase Inhibitors - May provide relief in women who have not had improvements with hormone therapy. Aromatase works by inhibiting the amount of estrogen the tissue can produce. Studies have shown that aromatase inhibitors are effective at reducing pain and preventing the return endometrial growths. This form of treatment is often used in conjunction with hormone therapy such as birth control pills or progestin.
Diagnostic Tests/Lab Tests/Lab Values
The following are common tests used to identify physical clues leading to the diagnosis of endometriosis:
- Laparoscopy: Accurate diagnosis of endometriosis requires direct visualization of endometrial tissue through laparoscopic procedures. This is accomplished by distending the abdomen through the injection of carbon dioxide for adequate visualization of the reproductive organs. An instrument with a camera (laparoscope) is inserted through a tiny incision near the navel in order to determine if reproductive and abdominal organs possess endometrial implants. Laparoscopy is a valuable tool guiding the course of treatment for endometriosis by identifying the severity, size and location of foreign implants.
- Pelvic Exam: Manual palpation of the pelvic region to identify abnormalities such as cysts or scar tissue surrounding reproductive organs. Although this exam may reproduce pain in large areas of implantation, it is often not possible to feel small areas, making this test less reliable at identifying the presence of endometriosis.
- Ultrasound: Ultrasounds work by using sound waves from a transducer wand to create a video image of organs. Vaginal ultrasounds are performed by inserting a wand into the vagina to view images of the reproductive organs, while abdominal ultrasounds are done by moving a wand over the abdominal-pelvic region. Ultrasound is done in order to identify the presence of cysts associated with endometriosis, but it is important to note that this is not a definitive test used to diagnose endometriosis.
- MRI: An MRI is used to view endometrial implants but proves to be more sensitive in comparison to the use of ultrasound.
- Blood Labs: Cancer antigen 125 (CA 125) is a blood test that has been used to detect common proteins found in those with endometriosis. This is the same test that is used to tumour markers for various types of cancer. Although this blood test may identify proteins in advanced cases of endometriosis, it is not sensitive to the detection of mild or moderates disease. Due to the fact that this test is not sensitive to early disease detection, it is not recommended as a screening test for endometriosis.
Medical Management
Endometriosis is a non-curable disease. The objectives of medical treatment focus on restoring normal pelvic anatomy, removal of endometriotic implants, and prevention of reoccurrence to decrease pain and increase fertility. In order to achieve these goals, the course of medical management depends heavily on the severity of symptoms, severity of disease, age and future child bearing plans. Generally, conservative treatment is recommended to control symptoms prior to surgical management.
Treatment Options
- Medications to control pain - (refer to medication section)
- Hormone Therapy - (refer to the medication section)
- Surgical management - less common approach due to unchanged aetiology and rapid implant regrowth.
- Non-traditional management - (refer to alternate/holistic management)
The main aspect of medical management is aimed at reducing or blocking ovarian function due to the fact that endometriosis is related to hormone function. Common medical treatments and their functions are listed in the medication section. In the instance that symptoms are severe and disabling, or conservative medical treatment fails, surgical procedures can be useful in removing/destroying implants and decreasing or ceasing symptoms. It is important to note that implant regrowth may occur following removal and may only be a temporary source of symptom relief.
Surgical Management
- Pelvic Laparoscopy/Laparotomy - Identifies implants for the diagnose endometriosis. Once identified, endometrial implants and/or scar tissue is removed using a digital laparoscope device for viewing and surgical tools for excision. Removal has been correlated with the success of conception and is indicated for those trying to become pregnant.
- Laparoscopic Cauterization - implants are destroyed using a cauterization probe. Indicated if endometriosis is mild with minimal adhesions.
- Laparoscopic uterine nerve ablation (LUNA) - indicated for patients experiencing intractable pelvic pain. This procedure works by interrupting pain-conducting neural pathways by destroying the efferent uterine sensory fibres in the uterosacral ligament as well as their secondary ganglia exiting the uterus. Uterine prolapse and ureter injury are secondary risk factors that may occur following this procedure.
- Total hysterectomy - removal of the uterus, both ovaries and fallopian tubes. Indicated for women 35 to 40 years of age who are disabled by pain, and do not wish to continue childbearing. Symptoms return in 1 out of 3 women who undergo partial hysterectomy's. Total hysterectomy has been shown to be the best surgical procedure in the hopes of curing endometriosis.
Physical Therapy Management
Preferred Practice Patterns
- 4C: Impaired Muscle Performance
- 4D: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated With Connective Tissue Dysfunction
Due to the fact that endometriosis is a common disease in women, physical therapists may encounter this as a primary diagnosis, co-morbidity, or possibly undiagnosed. It is important to be aware of the common signs and symptoms endometriosis presents with, especially those which mask as musculoskeletal.
The decision to treat patients diagnosed with endometriosis is based on the presentation of musculoskeletal and non-musculoskeletal symptoms. Patients with endometriosis may experience pain in the region of the pelvis, abdomen and low back. Secondary musculoskeletal impairments may occur in the region of endometrial implantation. For instance, endometrial implants on the psoas or lumbar musculature may reproduce musculoskeletal symptoms during the examination.
Secondary Musculoskeletal Impairments Caused by Endometriosis
- Lumbar, sacroiliac, and pelvic floor pain
- Muscle spasms
- Trigger points (common in the pelvic floor and lumbar spine)
- Connective tissue dysfunction
- Urinary urgency
- Scar tissue adhesion
Physical therapy may prove to be an integral treatment option for the patient with endometriosis presenting with musculoskeletal impairments. By addressing this disease using a multidisciplinary approach, decreased pain and increased functional capabilities may be provided, allowing for a greater quality of life.
Effective Physical Therapy Treatment Options
- Modalities
- Pelvic floor strengthening
- Internal and external trigger point management
- Myofascial manual therapy
- Stretching and flexibility exercises
- Spinal mobilizations
- Nerve glides
- Relaxation exercises
A study entitled Treating Fallopian Tube Occlusion with a Manual Pelvic Physical Therapy was performed in 2008 by Wurn, BF. et al. This study described the efficacy of a non-invasive soft tissue physical therapy treatment in opening bilateral occluded fallopian tubes in infertile women with a history of abdominal-pelvic adhesions. Through this study it was discovered that non-invasive therapy such as manual techniques may be useful as an adjunct therapy in treating tubal occlusion caused by adhesions.
Differential Diagnosis
The ability to differentiate between symptoms associated with pelvic disease remains an integral part of physical therapy examination and evaluation. It is important for physical therapists to complete a thorough examination to include standard screening procedures as well as auscultation for bowel and bruit sounds, palpation for masses, and percussion to assess the integrity of underlying abdominal structures. A number of primary musculoskeletal impairments can manifest as pelvic pain. Receiving a diagnosis of endometriosis may be a long process involving several different health care providers. Studies show that women typically see approximately nine different health care providers before receiving a definitive diagnosis of endometriosis. Below is a list of potential differential diagnoses to consider when evaluating a patient with abdominal, pelvic or low back pain.
- Dysfunction of the hip, spine, and/or sacroiliac joints
- Dysfunction of the anterior or posterior abdominal wall
- Gastrointestinal dysfunction
- Urinary tract dysfunction
- Pelvic inflammatory disease
- Ovarian cysts or tumours
- Obstructive anomalies