Clinically Relevant Anatomy
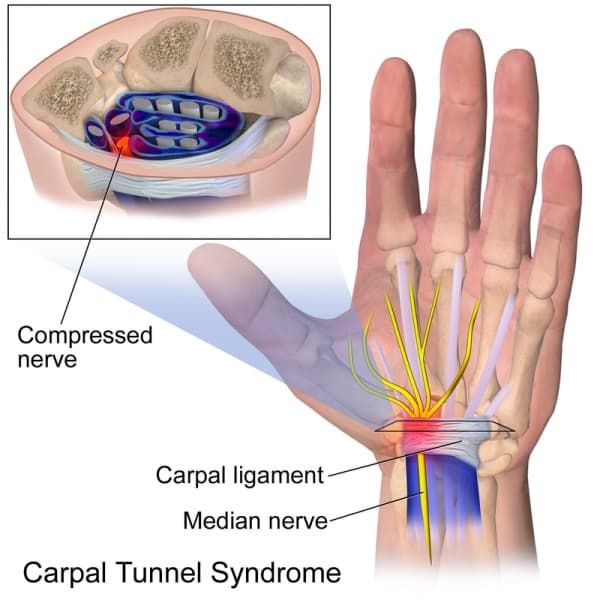
The carpal tunnel (CT) is formed by a non-extendable osteofibrous wall that forms a tunnel protecting the median nerve and flexor tendons. The wall of the tunnel consists of carpal bones, joint capsule, carpal ligaments, flexor carpi radialis tendon, and the flexor retinaculum. Carpal bones form an arch-like base for the tunnel. The flexor retinaculum which spans from the pisiform bone and the hamulus of the hamate bone to the scaphoid and the trapezium completes and closes the tunnel. The eight carpal bones are positioned in two rows between the ulna and radius and the metacarpal bones. These form an articulated connection between the forearm and the hand.
The CT allows the passage of multiple structures between hand and proximal segments of body. Tendons of flexor digitorum profundus, flexor digitorum superficialis and flexor pollicis longus muscles and the median nerve pass through the carpal tunnel. The median nerve passes from the forearm to the palmar aspect of the hand, Its sensory axons convey sensory stimulation for median nerve distribution consisting of the palmar aspect of thumb and fingers, except for the fifth digit and ulnar half of fourth digit. Motor axons of median nerve supply the muscles of thenar eminence.
Etiology and Epidemiology
The estimated prevalence of CTS is 4-5% of the population. There are two peak age frequencies: the first and biggest peak is between 45 and 59 years of which 75% is female. The second age peak is between 75 and 84 years, of which 64% is female. Most cases of CTS are idiopathic, A portion of incidences of CTS are caused by pathological changes in structures passing through the carpal tunnel or the tissues forming its walls. Finally, a considerable proportion of CTS cases are linked to pathological demands on wrist motion.
Idiopathic Carpal Tunnel Syndrome
- Idiopathic CTS occurs more frequently in females (65–80%), between the ages of 40 and 60 years; 50–60% of the cases are bilateral.
- The bilateral characteristic increases in frequency with the duration of symptoms.
- Idiopathic CTS is correlated with hypertrophy of the synovial membrane of the flexor tendons caused by degeneration of the connective tissue, with vascular sclerosis, edema and collagen fragmentation.[8] The histological changes were thought to be suggestive of dynamic factors as repetitive strain.
- Predisposing factors based on meta-analyses conducted in 2002 and 2008, include:
- Sex
- Age
- Genetic and anthropometric factors (size of the carpal tunnel) were of most importance followed by other correctable predisposing factors of clinical importance as:
- Obesity
- Smoking
- Excessive alcohol consumption
- Repetitive manual activities and exposure to vibrations and cold temperatures were the least important and of little clinical relevance
Secondary Carpal Tunnel Syndrome
Abnormalities of the Walls of the CT
- Any condition that modifies the walls of the carpal tunnel may cause compression of the median nerve.
- Abnormalities of the shape or position of the carpal bones: dislocation or subluxation of the carpus
- Abnormalities of the shape of the distal extremity of the radius: fractures (translation of more than 35%) or skewed consolidation of the distal radius; osteosynthesis material on the anterior face of the radius;
- Joint abnormalities: wrist arthrosis, inflammatory arthritis (due to synovial hypertrophy, bone deformation an/or carpal shortening), infectious arthritis, rhizarthrosis or villonodular synovitis
- Acromegaly.
Abnormalities of the Content of the CT
- Tenosynovial hypertrophy;
- Inflammatory tenosynovitis: inflammatory rheumatism lupus and infection
- Metabolic tenosynovitis: diabetes mellitus (abnormality of collagen turnover), primary or secondary amyloidosis (chronic hemodialysis with deposition of beta-2-microglobulin), gout and chondrocalcinosis;
- Abnormalities of fluid distribution: pregnancy in 0.34% to 25% of the cases, especially in the third trimester, with frequent signs of deficit in 37–85% of the cases; hypothyroidism and chronic kidney failure (arteriovenous fistula).
- Abnormal or supernumerary muscle: deep palmar muscle intra-tunnel position of the muscle body of the superficial flexor or proximal extension of the muscle body of the lumbrical muscles
- Persistent arterial hypertrophy of the median nerve
- Intratunnel tumor: lipoma, synovial cyst, synovial sarcoma or neural tumor (schwannoma, neurofibroma or lipofibroma);
- Hematoma: hemophilia anticoagulant accident or trauma
- Obesity
Dynamic Carpal Tunnel Syndrome
The pressure inside the carpal tunnel increases during wrist extension and flexion Repetitive extension and flexion movements of the wrist, along with flexion of the fingers and supination of the forearm, have been implicated in this increase Incursions of muscle bodies from the superficial and deep flexors of the fingers, when the wrist and fingers are extended, have been found in 50% of the cases This particular movement can be seen in occupational pathological conditions
Computer Work and CTS
No increase in the prevalence of CTS in cases of working on computers for more than 15 h per week has been observed. A tendency toward increased prevalence has been demonstrated in cases of working on computers for more than 20 h per week
Clinical Presentation
CTS onset is generally gradual with tingling or numbness in the median nerve distribution of affected hand.
Patients may notice aggravation of symptoms with static gripping of objects such as a phone or steering wheel but also at night or early in the morning. Many patients will report an improvement of symptoms following shaking or flicking of their hand.
As the disorder progresses, the feeling of tingling or numbness may become constant and patients may complain of burning pain.
The final symptoms are weakness and atrophy of muscles thenar eminence. These combined effects of sensory deprivation and weakness may result in a complaint of clumsiness and loss of grip and pinch strength or dropping things,
Differential Diagnosis
The process of differential diagnosis should give consideration to all conditions which could potentially cause a dysfunction of the median nerve, or its contributories in brachial plexus, C 5 to 8 nerve roots and central nervous system. For example. an injury of nn. digitales in the palm, pronator teres syndrome or cervicobrachial syndrome, particularly when C7 nerve root is involved. Even though the neurological symptoms of this pathology have a distinct dermatomal character, the C7-C8 dysfunction with radiculopathy will overlap with CTS in the location of paraesthesia of hand.
Other conditions to be aware of when diagnosing CTS include:
- Neuralgic amyotrophy.
- Intracranial neoplasms
- Multiple sclerosis
- Cervical syringomyelia
- Brachial plexus injury
- Pancoast tumor
Diagnostic Procedures
Electroneuromyography (ENMG) examination is used to examine the sensory and motor nerve conductance of the median nerve. It also highlights the elective weakening in passing through the carpal tunnel. It is considered abnormal when there is a diminished sensory conduction velocity between the wrist, the palm of the hand and the fingers. This test may be used to diagnose the condition and rule out other pathologies.
Electromyogram (EMG) of the muscles innervated by the median nerve measures electrical discharges produced in the muscles. This test can determine if there is any muscle damage and can rule out other conditions.
Ultrasonography can identify space-occupying lesion in and around the median nerve. The test can confirm abnormalities that can diagnose CTS and help guide steroid injections into the carpal tunnel.
X-ray is recommended to exclude other causes of wrist pain like arthritis or bony pathology.
Outcome Measures
There are several questionnaires available to determine the outcome measures for CTS.
Medical Management
Non-surgical treatment comprises oral steroids, corticosteroid injections , NSAID, diuretics, vitamin B6 and splinting/hand brace.
Reviews show that there is moderate and strong evidence for the effectiveness of curing CTS using oral and local steroids. Huisstede et al says that for both treatments no evidence was found for long term effectiveness. Diuretics, NSAID and vitamin B6 turn out to be ineffective. There is limited to moderate evidence of the effectiveness of splinting in short-term. Huisstede et al claim that the number of nonsurgical interventions benefits CTS in the short term, but there is sparse evidence on the midterm and long-term effectiveness of these interventions
Huistede et al concluded that surgical treatment seems to be more effective than splinting and anti-inflammatory drugs plus hand therapy in the midterm and long term to treat CTS. However, there is no unequivocal evidence that suggests one surgical treatment is more effective than the other.
The two main manners to decompress the median nerve by surgery are the open carpal tunnel release (OCTR) and the endoscopic carpal tunnel release (ECTR). During the OCTR the 2 cm incision is performed through skin, palmar fascia to access and release the transverse carpal ligament. The less invasive ECTR minimises the size of skin incision while releasing the transverse ligament. During this operation, the surgeon can use the single-portal technique and the two-portal technique. The first technique uses one incision, the second one, two. Using a camera, surgeons can see what happens inside.
Benson et al state that with both techniques (OCTR and ECTR) the structural complications for nerves, blood vessels or tendons are low. According to Chen et al there are no obvious statistical differences in relief of symptoms (pain en paraesthesia), recovery of grip strength a reoperation rate. Though, two articles with moderate to strong level of evidence state the ECTR causes a faster return to work and a better recovery of pinch strength.
Physical Therapy Management
Patients with mild to moderate symptoms do not need to be immediately operated but can be effectively treated in a primary care environment Physical therapy typically consists of modifications of activities and the workplace (ergonomic modifications) , patient education, carpal bone, and nerve mobilisation , ultrasound and electromagnetic field therapy and splinting.
It’s important to mention that, in general, the evidence of the effectiveness of the exercise and mobilization interventions is limited and very low in quality. The physical therapist should always inform the patient about the limited evidence of effectiveness and safety as well as the availability of surgical options without the pre-requite conservative therapy where appropriate.
The effectiveness of ultrasound varies between the studies and most of the time the evidence is low. According to Page et al there’s poor and limited evidence about the effect of therapeutic ultrasound. There is insufficient evidence that therapeutic ultrasound has a greater benefit than other non-surgical treatments, such as splinting, exercises or oral drugs.
It is important to pay attention to the cause of the CTS. Physical therapists should give advice in task modification, like taking sufficient rest and variation of movements. Burke et al declare that often simple obvious alterations to the working practice can be beneficial in controlling milder symptoms of CTS.
Peter et al declare that evidence about post-operative rehabilitation is also limited. Their reviewed interventions handle physical applications, differences between kinds of immobilisation and multimodal hand therapy. None of them seems to have a prevailing benefit.
Clinical Bottom Line
Patients may benefit from physiotherapy based treatment with goals of CTS symptom reduction and functional gains, provided that:
- Their symptoms are intermittent and not rapidly worsening or if their CTS etiology is highly suggestive of the possibility of remission as an example of pregnancy-related CTS
- Patients are informed about the lack of high-quality evidence for the effectiveness and safety of therapeutic modalities used by physiotherapists,
Treatment should be discontinued when shown to be ineffective and appropriate, evidence-based discharge recommendations should be made.
CTS symptoms typically escalate over a longer-term despite conservative treatment. Surgical interventions for appropriate patients have been shown to be safe and more effective than any conservative intervention, Clinicians should be aware that constant tingling or numbness is associated with significant compression of the median nerve. Prolonged duration of such symptoms may lead to irreversible changes in its internal structure, affecting the effectiveness of surgery and leaving individuals with chronic symptoms and muscle atrophy of thenar eminence. Patients should be followed by their general practitioners to discuss surgical treatment options when necessary and desired.